PQRST Pain Assessment Method
The PQRST mnemonic is a valuable tool for pain assessment when responding to medical emergencies.
You can use it to gather information about the patient’s symptoms and level of pain. It can help you devise an effective pain management plan and start much-needed treatment immediately.
In this post, we’ll explain how to use the PQRST mnemonic to assess pain effectively during a first aid response.
At firstaidforfree.com we love our first aid mnemonics and we’ve tried to compile a list of the best first aid mnemonics around.
What Does PQRST Stand For?
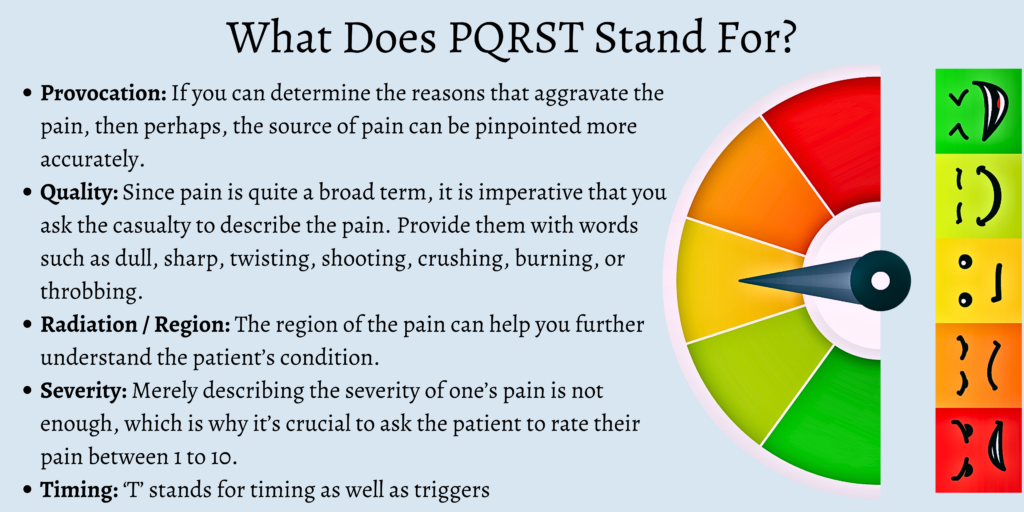
PQRST is a pain assessment method that stands for:
Provocation
Quality
Radiation / Region
Severity
Timing
Now, let’s take a closer look at each factor.
Provocation or Palliation
If you can determine the reasons that aggravate the pain, then perhaps, the source of pain can be pinpointed more accurately. Ask the patient what they were doing when the pain first started, what the triggers are, and if certain activities or positions that worsen the pain.
A patient may feel pain for obvious reasons, such as a medical condition or a physical injury. When the cause of pain is unknown, the first thing to investigate is what provokes it.
Your goal is to determine whether certain activities, movements, and positions worsen the pain. Consider asking these questions:
- Do specific actions or movements aggravate pain? (e.g., standing, walking, stretching, laughing, coughing, deep breathing, etc.)
- Does external pressure worsen or relieve the pain?
- Is the pain worse or relieved in certain positions? (e.g., sitting, standing, lying flat, lying on the side, etc.)
In addition, you want to know if the patient has made initial attempts at pain relief.
- Have you taken any pain medications? Did it help?
- Have you tried any at-home treatment to ease the pain? (e.g., hot or cold compress, massage, herbal oils, etc.) Did it work?
Quality
Since pain is quite a broad term, it is imperative that you ask the casualty to describe the pain. Provide them with words such as dull, sharp, twisting, shooting, crushing, burning, or throbbing.
For example, if they have chest pain, it could point to a cardiac condition, and if they feel pain in their nerves, it will probably be more focused and sharper.
Ask the patient to describe their pain. If the patient cannot explain their symptom, offer these adjectives:
- Sharp
- Shooting
- Dull
- Throbbing
- Burning
- Aching
- Cramping
- Agonizing
Region or Radiation
The region of the pain can help you further understand the patient’s condition. There can be two types of pain, namely radiating pain and referred pain.
Radiating pain keeps spreading from the pain’s point of origin. An example of this is when one’s sciatic nerve gets pinched.
Referred pain is when someone experiences pain in a location that is different from the actual source of the issue. The most common example is the ‘brain freeze’ we might experience on having ice cream.
So, ask them where the pain is located and if it radiates. It is also vital to find out if they feel like it has been traveling around or if they feel it started at one point and is now localized at a different spot.
The location of the pain narrows down the conditions the patient may have. Another clue is radiating pain, where pain spreads into a broader area of the body.
For example, cardiac chest pain can radiate to the arms, back, and jaw.
Here are some guide questions to keep in mind:
- Where do you feel the pain?
- Is it confined to just one part?
- Does it travel or spread to other areas?
- Did it start in one spot and is now in another place?
Note: you can ask the patient to point to the location of the pain.
Severity
Merely describing the severity of one’s pain is not enough, which is why it’s crucial to ask the patient to rate their pain between 1 to 10.
Ask them the following questions as well:
- How bad is the pain when it’s at its worst?
- Does the pain interfere with any other activities?
- How long does every episode last?
- Does it force you to lie down or slow down or sit down?

Timing
‘T’ stands for timing as well as triggers. The questions in this category include:
- When or at what time did the pain begin?
- Is the pain gradual or sudden?
- How often does the pain occur?
- How long does the pain last?
- At what time of the day do you usually experience pain?
- Does the pain ever wake you up?
- Has the pain ever led to anything else?
- Do you feel the pain before, after, or during your meals?
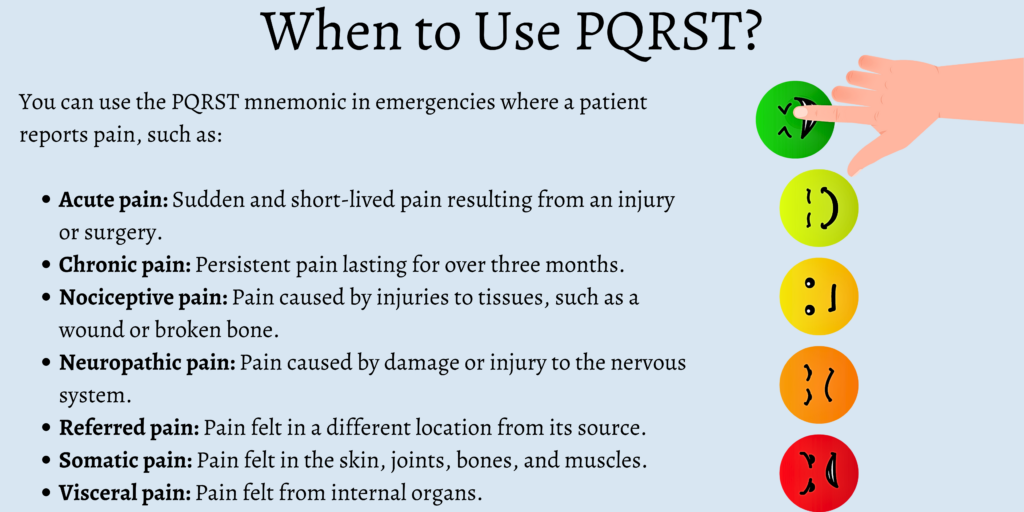
When to Use PQRST?
You can use the PQRST mnemonic in emergencies where a patient reports pain, such as:
- Acute pain: sudden and short-lived pain resulting from an injury or surgery
- Chronic pain: persistent pain lasting for over three months.
- Nociceptive pain: pain caused by injuries to tissues, such as a wound or broken bone
- Neuropathic pain: pain caused by damage or injury to the nervous system
- Referred pain: pain felt in a different location from its source
- Somatic pain: pain felt in the skin, joints, bones, and muscles.
- Visceral pain: pain felt from internal organs
Example Situations
The PQRST mnemonic can be effective in documenting chest pain. Check out this example:
- Provocation: The pain started after climbing a flight of stairs. It gets worse with activity.
- Quality: The pain is crushing.
- Radiation: The pain is on the left side of the chest and spreads to the neck, back, and shoulders.
- Severity: The pain is an 8 out of 10.
- Timing: The pain lasts several minutes, goes away, and returns.
This example uses the PQRST mnemonic to assess abdominal pain:
- Provocation: The pain started after eating a large meal. It worsens when coughing or laughing.
- Quality: The pain is a constant dull ache.
- Radiation: The pain radiates to the back.
- Severity: The pain is a 6 out of 10.
- Timing: The pain has been present for an hour and has not improved.
In each of these situations, the first-aider quickly gathers vital information about the patient’s pain that can help guide treatment.
Other Questions to Ask for Further Assessment
Here are a few more questions to ask a patient to evaluate their pain:
- Do you have any symptoms aside from pain?
- Are you taking any medications?
- Do you have any allergies?
- Do you have any history of recurrent pain?
- Did you have a recent accident or surgery?
FAQs
What is the full form of the acronym PQRST as a pain assessment method?
‘P’ stands for provocation, ‘Q’ is for quality, ‘R’ means radiation or region, ‘S’ means severity, and ‘T’ stands for timing
What are some of the adjectives with which a patient can describe their pain?
A couple of the adjectives that patients can resort to in order to describe their pain include twisting, shooting, nauseating, burning, stabbing, dull, and sharp
In terms of location, what are the two types of pain that can exist?
When it comes to narrowing down the region of the pain, the two kinds of pain could be referred to as pain and radiating pain.
How can you find out the severity of a patient’s pain?
You can find out how severe a patient’s pain is by asking them to rate it between 1 to 10.
Final Thoughts
In conclusion, the PQRST mnemonic is a systematic approach to understanding a patient’s pain. This method can help the first-aid provider capture crucial details about the symptom quickly and accurately, facilitating intervention
Want to learn more about first aid? Why not take one of our free online first aid courses! No registration or certificate fees.




Very informative
Thank you!
Great read
Thank you!
Very impressive
Thank you!
Thanks