Is Cyanosis an Emergency?
Cyanosis is a condition in which a person’s skin, nails, or lips turn blue. It signifies that the patient’s muscles, organs, and tissues aren’t receiving the adequate quantity of blood required to function effectively.Several different medical conditions can lead to cyanosis, such as ones related to a patient’s heart, lungs, and central nervous system. Although a blue hue on the lips and skin isn’t always concerning, certain conditions could call for emergency medical attention.
What is Cyanosis?
Cyanosis is a blueish/purple tinge to the skin caused by tissues receiving a poor supply of oxygen rich blood. It is a pathologic sign, otherwise known as a symptom, and not a disease in and of itself. Generally speaking, a patient with underlying conditions that cause the deoxygenated hemoglobin level to raise to 5.0 g/dl or more will display Cyanosis. Cyanosis can be observed most apparently in areas of the body with high vasculature, which is why it is common to see Cyanosis of the lips and gums.
Is it an Emergency?
First off, Cyanosis can be caused by many different conditions, some of which may be an indication of a serious medical condition. It is important to determine the cause of Cyanosis in order to understand if this symptom is an emergency and how urgently you should seek medical attention. MostBut if you see a sudden change, like an adult or child suddenly turning blue, then please seek medical attention immediately.
What Does Cyanosis Look Like?
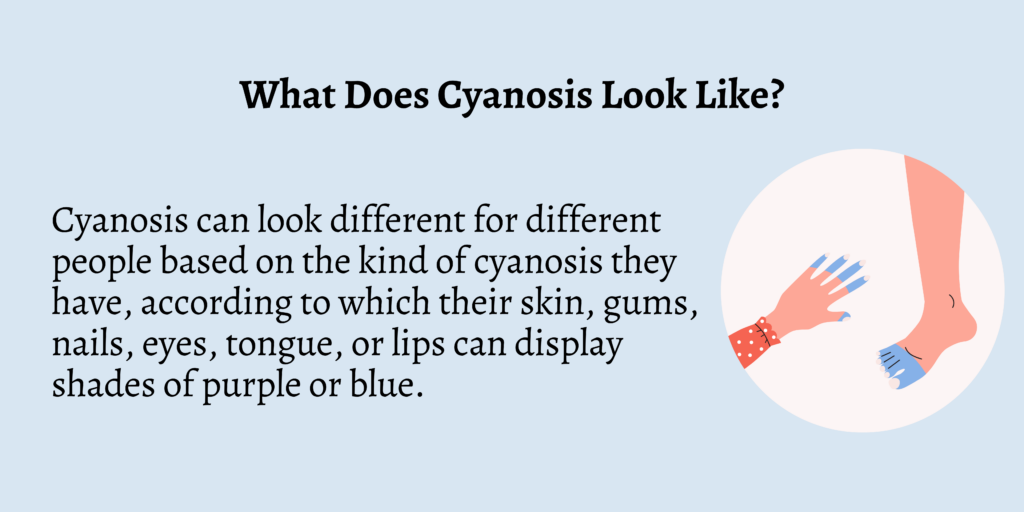
Cyanosis can look different for different people based on the kind of cyanosis they have, according to which their skin, gums, nails, eyes, tongue, or lips can display shades of purple or blue.
When a person has darker skin, cyanosis can give their skin a gray or white appearance.
What are the three types of Cyanosis?
There are three different types of Cyanosis: central, peripheral, and circumoral (perioral). Central and Peripheral Cyanosis
Central Cyanosis
Central Cyanosis is caused by arterial hypoxia − where there is a low level of oxygen in the red blood cells leaving the heart. This is a late sign in trauma but can also be caused, for example, by congenital heart defects or lung failure, which can lead to both slow blood flow and low oxygen in the blood. It is important to seek medical attention immediately.
Peripheral Cyanosis

Peripheral cyanosis is rarely a life-threatening emergency, and is most commonly caused due to the reduction of blood flow in the peripheral circulation. This blue skin can be due to vasoconstriction caused by cold or shock, where not enough oxygen rich blood is reaching the extremities, but leaving the heart normally perfused. Peripheral cyanosis is found in the distal extremities (hands and feet, fingertips and toes). The picture in this post shows an example of peripheral cyanosis.
Circumoral (Perioral) Cyanosis
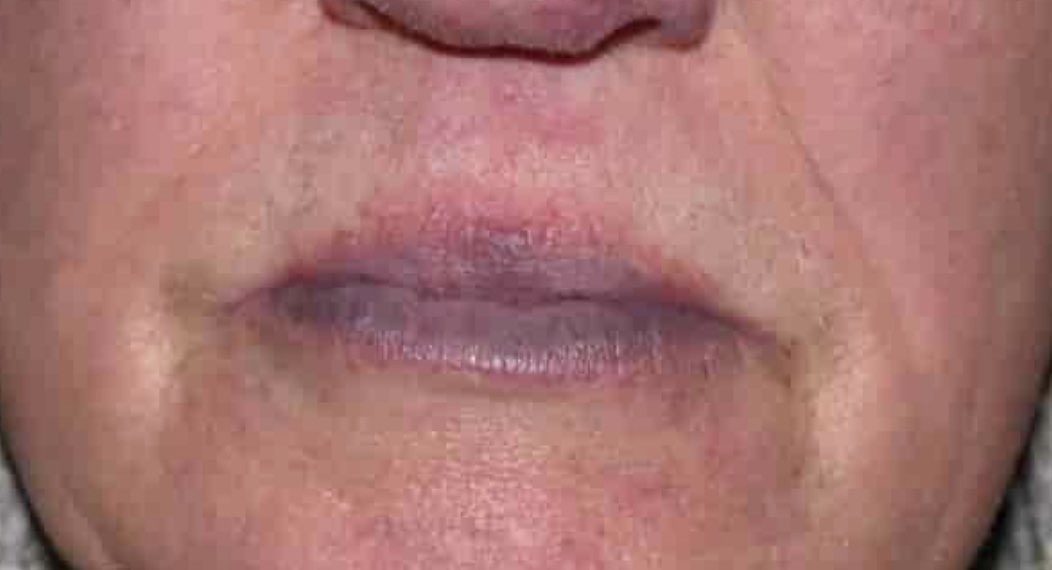
This is bluish discoloration of the mouth or the lips, and other mucous membranes. It is most commonly caused by constricted blood vessels in response to cold temperatures. However, blue discoloration of the lips on an infant can be a sign of a blocked airway, which is an emergency that may require immediate medical treatment. On dark-skinned patients, Cyanosis may be harder to detect, in which case Circumoral Cyanosis may be the most apparent symptom.
How to Detect Cyanosis?
An absence of cyanosis does not indicate that the patient is not hypoxic − for example, low light levels and some artificial lights can simply make cyanosis hard to detect. A pulse oximeter can be used to more accurately assess the whether a patient is hypoxic or not.
Cyanosis may be apparent on your physical examination and assessment of the patient and can be caused by a number of medical emergencies. It is important for first aiders to be able to spot cyanosis and hand over this information to emergency medical staff.
Cyanosis Causes in Adults
Some common causes of cyanosis in adults may include:
- Respiratory Problems: conditions affecting the ability of the lungs to enrich oxygen in the blood through carbon dioxide exchange. These may include Emphysema, Pneumonia, Asthma, Chronic Obstructive Pulmonary Disease (COPD), or even a blood clot in an artery of the lung.
- Airway Problems: such as choking, swelling or inflammation of the airway.
- Cardiovascular Problems: these may include congestive heart failure or a heart attack, both of which affect the body’s blood flow and ability to deliver oxygen rich blood.
- Blood Disorders: any condition that interferes with the body’s ability to transport oxygen in the blood, like sickle cell anemia.
- Exposure to Substances: exposure to gold and silver salts may cause cyanosis.
- Other causes: these may include but are not limited to blood flow that is limited by tight clothing, seizures, medications used to treat high blood pressure, and drug overdose.
Cyanosis Causes in Newborns
Some common causes of cyanosis in newborns may include:
- Respiratory Distress: a newborn that has difficulty breathing may have a bluish tinge to the skin and mucous membranes
- Congenital Heart Defects: problems with the heart that are present at birth
- Anemia: if the infant has a low bed blood cell count, lowering oxygenated blood flow
- Infections: Sepsis or meningitis may both alter the newborns ability to deliver oxygen rich blood
- Cold Exposure: this may cause peripheral cyanosis or circumoral cyanosis in newborns
Tests to Diagnose Cyanosis
The following are some of the tests that can help in diagnosing cyanosis:
- Chest X-ray
- Complete blood count (CBC)
- Cardiac catheterization to diagnose the state of a person’s heart
- Electrocardiogram
- CT scan
- Pulmonary function tests to identify the patient’s lung condition
- Arterial blood gas analysis to check how much oxygen is present in the arteries along with other substances
- Echocardiogram
- Pulse oximetry to check the oxygen present in the patient’s blood
Cyanosis Treatments
It’s important to identify the cause of Cyanosis before treatment can be administered. This can entail administering oxygen, addressing any metabolic issues, performing surgery, or administering medications to treat particular medical disorders. Sometimes, making lifestyle adjustments like giving up caffeine or smoking can be beneficial. Depending on the severity of Cyanosis, treatment in a hospital or other medical facility may be warranted.
- Oxygen support: if the cyanosis stems from an issue with the lungs or heart, the person may need to be given oxygen through a nasal cannula or assisted ventilator (a machine that helps them breathe).
- Correction of metabolic abnormalities: If the cyanosis is caused by more general problems with the body’s metabolism (the way it processes substances like sugar and minerals), the person may need to be given medications to correct these problems. Hypoglycemia and hypocalcemia in particular should be corrected before other treatments are given.
- Treatment of specific health conditions: If the cyanosis is caused by a specific health condition like a heart defect, the person may need to see a specialist (like a cardiologist) and receive treatment such as surgery or medications.
- Lifestyle changes: In some cases, making longer-term changes to the person’s lifestyle (like quitting smoking or avoiding caffeine, which both constrict blood vessels) may be helpful in reducing cyanosis.
Want to learn more about first aid? Sign up to one of our free online training classes today!
What to Expect in Cyanosis?
If a person has cyanosis, the time it takes for them to get better depends on the type of cyanosis and the speed at which they avail the necessary treatment.
It’s not usually a life-threatening condition, but one must consult a doctor if they display any of the symptoms or if the condition occurs when they’re at rest or warm.
How to Prevent Cyanosis?
Cyanosis can be caused due to various reasons, and there isn’t much a person can do to prevent them all. However, certain measures can be taken as precautions. For example, your doctor could ask you to stop consuming the medicines that restrict blood flow.
You should also reduce your consumption of caffeine and quit smoking. You must ensure to wear warm clothes in colder climates so that your toes, fingers, nose, and ears stay protected.
FAQs
1. What happens when you have cyanosis?
When a person has cyanosis, their skin, lips, or nails turn blue or purple.
2. Are there different types of cyanosis?
Yes, there are three different types of cyanosis, namely central, peripheral, and perioral/circumoral cyanosis.
3. What are the tests done to diagnose cyanosis?
The tests done to diagnose cyanosis include chest X-ray, CT scan, echocardiogram, and electrocardiogram.
4. What are the various symptoms of cyanosis?
Apart from one’s skin turning blue, some of the other symptoms of cyanosis are coughing, dizziness, weakness, and low body temperature.
Conclusion
Cyanosis can be caused due to heart problems, lung issues, or even problems related to the airway. By being aware of the symptoms involved for both kids and adults, you can get the required treatment immediately.
If you witness bluish skin on yourself or anyone around you, call the emergency medical services immediately.