What are the Common Causes of Hypoxia?
Hypoxia is a medical condition that is caused by restricted blood flow or a reduced oxygen level in the blood.
These are the risk factors of hypoxia one should know about:
Anyone who suffers from lung or heart issues such as asthma is at a higher risk of getting hypoxia.
Another factor that multiplies the risk of hypoxia is infections, such as influenza and pneumonia.
Are hypoxia and hypoxemia the same thing, you might ask? Although hypoxia and hypoxemia sound similar, they cannot be used interchangeably. Hypoxia refers to low oxygen levels in your body’s tissues. Hypoxemia is when your blood has low levels of oxygen.
In this article, we will be discussing the causes of hypoxia, how it is diagnosed, and much more.
What is Hypoxia?
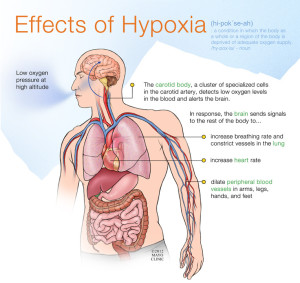
Hypoxia is a state or condition in which the tissues or cells in a human body don’t receive enough oxygen to function properly.
Here is what happens when we breathe in and breathe out:
- When we inhale, our lungs take in oxygen from the air.
- This oxygen is then transferred to our blood.
- The blood then takes this oxygen to our cells and tissues.
- The oxygen enters the cells, and this is where the exchange with carbon dioxide takes place.
- As we exhale, the carbon dioxide gets removed through the lungs.
When we don’t get enough oxygen at any point during this entire process, it could cause hypoxia. The flow of blood and the flow of air are both significant for the process, which is why heart disease and lung disease can both increase your chances of suffering from hypoxia.
Outside the body
Environmental changes can cause hypoxia if the amount of oxygen in the air is reduced:
- Smoke
- Gas / Carbon Monxoide
- High altitude
- Deep sea
- Mine shafts
- Tunnels
- Depressurised aircraft
Obstruction of the upper airway
Patients who have a reduced level of consciousness are particularly vulnerable to upper airway obstruction.
- Tongue – this is the most common cause!
- External blockage (eg plastic bag)
- External pressure on the neck
- Drowning
- Blood / vomit
- Inhaled objects (eg food)
- Facial / neck injuries
- Internal swelling of the throat – stings (Anaphylaxis) / burns
Chest or lung trauma
- External compression – crowds, sand, damaged vehicle
- Rib fractures
- Blast injuries
- Pneumothorax (air in the thoracic cavity)
Paralysis of respiratory nerves and muscles:
- Electrocution
- Head and/or spinal injuries
- Stroke
- Drugs
- Chronic muscular diseases
- Some poisons such as weed killers and nerve gases
Internal lung problems:
- Chronic Obstructive Pulmonary Disease (COPD)
- Pneumonia / Lower Respiratory Tract Infections
- Asthma
Types of Hypoxia
The following are the different types of hypoxia:
1. Hypoxemic Hypoxia
Hypoxemic hypoxia occurs when your blood has an insufficient amount of oxygen, due to which the vital organs and tissues in your body don’t receive enough oxygen.
2. Hypemic (Anaemic) Hypoxia
Hypemic or anaemic hypoxia takes place when anaemia (the lack of healthy red blood cells) is the reason that your blood doesn’t carry enough oxygen. This leads to your tissues not having sufficient oxygen to function effectively.
3. Stagnant (Circulatory) Hypoxia
Stagnant or circulatory hypoxia occurs when your body’s tissues don’t receive enough oxygen due to poor blood circulation. This can either happen throughout your body or just in one area.
4. Histotoxic Hypoxia
Histotoxic hypoxia is the state where even though your blood has enough oxygen and the blood flow is proper, your tissues can still not use the oxygen efficiently.
How to Diagnose Hypoxia?
If your healthcare provider suspects you have hypoxia, they will:
- Conduct a physical examination.
- Check your skin, lips, and nails to see if they appear bluish in colour.
- Check your oxygen levels by asking you to get some tests done so as to find out the underlying cause of hypoxia.
Some of the tests that help in diagnosing hypoxia are:
- Imaging tests: Imaging tests like CT scans and X-rays help in getting images of a person’s internal organs, which can help in detecting the cause of hypoxia.
- Pulse oximetry: Your blood’s oxygen level gets measured by attaching a sensor to your body.
- Arterial blood gas test (ABG): Your oxygen levels are checked by drawing blood using a thin needle from your arm, wrist, or groin.
- Arterial blood gas test (ABG): This test is to see how well your lungs function, and it’s done by blowing out and breathing into a mouthpiece linked to a machine.
- Echocardiogram (ECG): An ECG is an ultrasound that checks how well your heart is working and helps in diagnosing the causes of hypoxia.
- Electrocardiogram (EKG): An EKG is a non-invasive procedure that checks for irregular heartbeat or signs of heart damage.
How to Prevent Hypoxia?
Since hypoxia occurs unexpectedly, it’s not really possible to prevent it. However, there are certain steps you can take to prevent hypoxic episodes from occurring, and those steps include:
- Follow all the safety guidelines and use the required equipment whenever you engage in high-risk activities or work in high-risk environments.
- If you’re travelling in a region with high altitudes, take precautions so that your body has enough time to adjust to the reduced level of oxygen. Avoid vigorous exercise and stay hydrated till your body gets used to the higher altitude.
- If you suffer from a cardiovascular or respiratory disease, follow your treatment plan strictly so as to prevent the complications that could cause hypoxia.
FAQs
What are the signs of hypoxia?
Some of the signs of hypoxia are restlessness, confusion, difficulty in breathing, and having bluish skin.
How long does hypoxia last?
The duration of hypoxia can vary depending on how severe it is, and at times, it can last for months.
Does hypoxia show up through an MRI scan?
Yes, an MRI scan can be useful in detecting hypoxia.
Why is hypoxia worse at night?
Hypoxia causes issues with a person’s night vision. This is because the cells in the eye that give us our night vision need a lot of oxygen. When they don’t receive that oxygen, it impairs their vision.
How long does it take to recover from hypoxia?
The first six months are crucial for a person’s recovery from hypoxia. After a year, you can determine what the long-term outcome could be.
Conclusion
Here are the key takeaways from the article to remember:
- Although hypoxia is a life-threatening condition, it can be treated if the patient is given proper and immediate medical care.
- The symptoms of the condition vary from one person to another. Whether you have severe hypoxia or long-term and mild hypoxia, it can still cause a lot of severe damage.
- Therefore, it is vital to get the necessary treatment and get in touch with your healthcare provider if you experience any worrying symptoms.