What Does TWELVE FLAPS Stand For?
TWELVE FLAPS is a memory device (also called a mnemonic) used to assess a casualty’s airway and breathing. This easy-to-remember acronym is often taught to paramedics and ambulance staff, but it’s also a useful and potentially life-saving tool for first aiders and first responders.
Assessing a casualty’s breathing is essential, and the results of the assessment can help to inform us about a patient’s condition and what actions need to be taken next.
But in a high-pressure emergency situation, remembering the steps you need to take to carry out a thorough and accurate assessment can be difficult. Thankfully, the TWELVE FLAPS memory device has been designed to walk you through the process step by step.
What Each Letter of The TWELVE FLAPS Stands For?
TWELVE
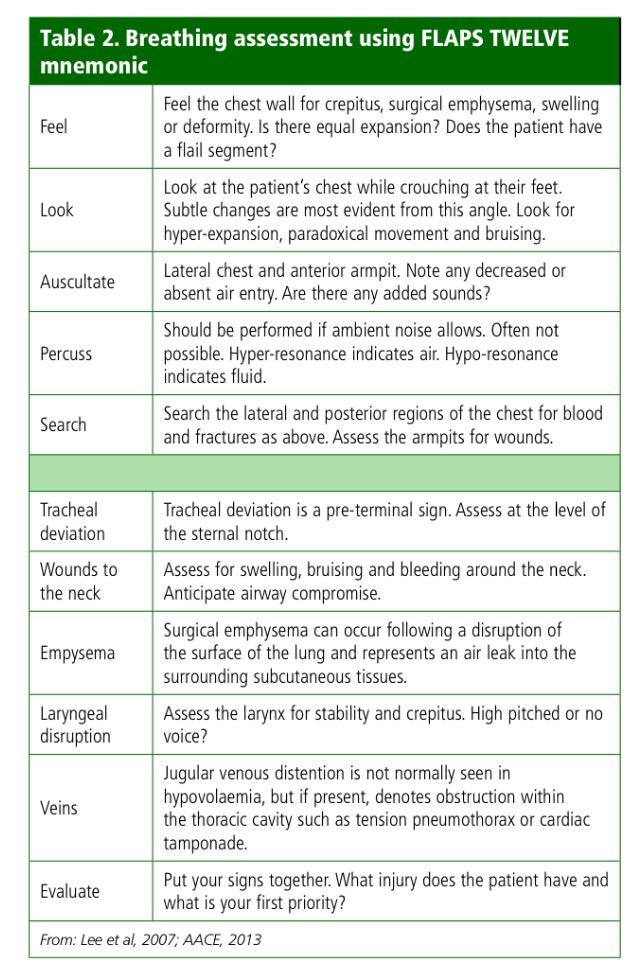
The TWELVE component lists some common signs to look out for when performing an examination of a casualty’s chest:
T – Tracheal deviation
W – Wounds and bleeding
E – surgical Emphysema
L – Laryngeal crepitus/injury
V – distended neck Veins
E – Expose and examine the chest
FLAPS
The FLAPS component shows us the methods we need to use to assess the chest, looking for the signs listed above.
F – Feel
L – Look
A – Auscultate
P – Percuss
S – Search the sides and back
The TWELVE FLASP Component
Lets dive in for detailed explanation
Tracheal Deviation
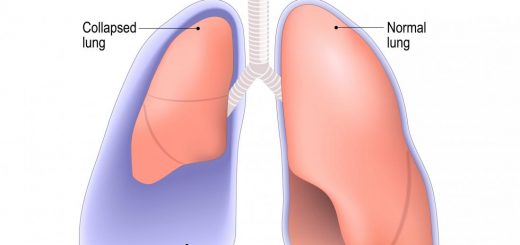
Look and feel for the location of the trachea. A displaced or deviated trachea can indicate a pneumothorax, a potentially life-threatening condition where excess air is trapped between the lungs and the chest wall.
Assess the level of the sternal notch, located at the top of the sternum, by looking and feeling.
Wounds to the Neck
Search the neck for any wounds, bruising, swelling, or bleeding. Pay close attention to any signs of damage to the airway or factors that may compromise a casualty’s breathing, such as a puncture wound.
Emphysema
Surgical, or subcutaneous, emphysema is often caused by a disruption or injury to the surface of the lung, which causes air to leak into the subcutaneous tissues.
Check the signs of this condition by looking for swelling and feeling and auscultating (listening) for crepitus (a popping or crackling sound that can be heard upon touching the skin.)
Laryngeal Disruption
A disrupted larynx can compromise the airways. Assess the larynx for stability and crepitus. Look for evidence of injury or deformity, and auscultate (listen) for signs of a high-pitched voice or a loss of voice.
Veins
Look for an engorged or distended jugular vein. This could be a sign of a potentially fatal obstruction in the thoracic cavity; for example, a tension pneumothorax (trapped air in the pleural space which compresses the lungs and other organs) or cardiac tamponade (a build-up of pericardial fluid which compresses the heart.)
Note that an engorged or distended jugular vein is not normally seen in hypovolemia (a lack of fluid such as blood or water in the body.)
Evaluate
Now that you have assessed the patient for all of the relevant signs evaluate the information and use it to decide what to do next. Does the patient have an injury, abnormality, or deficit that is affecting their breathing? If so, what is your first priority?
Feel
Using our hands to feel the chest wall can help to inform us about the quality of a patient’s breathing. It can also help to identify any swelling, deformities, crepitus, flail segments (broken ribs), or subcutaneous emphysema (a condition where air becomes trapped inside the subcutaneous layer of skin.)
Check that air is entering both lungs equally by feeling the rise and fall on each side.
Look
Look at the patient’s chest by crouching at their feet. Subtle changes are more evident from this angle.
Again, check that air is entering both lungs equally by observing the rise and fall of the chest wall.
Also, look for visible signs of bruising or other injuries or deformities. Check for hyper-expansion (barrel chest) and paradoxical breathing, a condition where the chest wall moves in the opposite direction of normal breathing movement.
Auscultate
Auscultation refers to listening to the sounds of the chest to detect any abnormalities in the lungs or other organs. Listen laterally from one armpit to the other, paying attention to any decreased or absent air entry and any additional sounds such as wheezing, crackling, popping, or crepitus.
Percuss
Percussion is the action of tapping on a patient’s chest to audibly identify normal resonance, hyper-resonance, or hypo-resonance.
This is often not possible in an emergency situation, as background noise may drown out any clues you might otherwise be able to hear. But if the ambient noise allows, percussion is a useful tool.
Hyper resonance may indicate an over inflation of air in the lungs. Hypo resonance may indicate a build of fluid, such as blood or water, in the lungs.
Search
Carry out a thorough search of the patient’s chest, both laterally (from the side) and posterior (from the back), including a thorough check of the patient’s armpits. Only move the patient to examine the back of the chest if it is safe to do so.
During your search, check for blood and signs of fractures, wounds, and other deformities.
Conclusion
By memorizing the TWELVE FLAPS, you will be much better prepared to assess a casualty’s airways and breathing in a first aid situation. This knowledge is vital, as taking quick action to identify and locate an obstruction could save someone’s life. To find out more about the anatomy of the respiratory system, read our in-depth guide here.