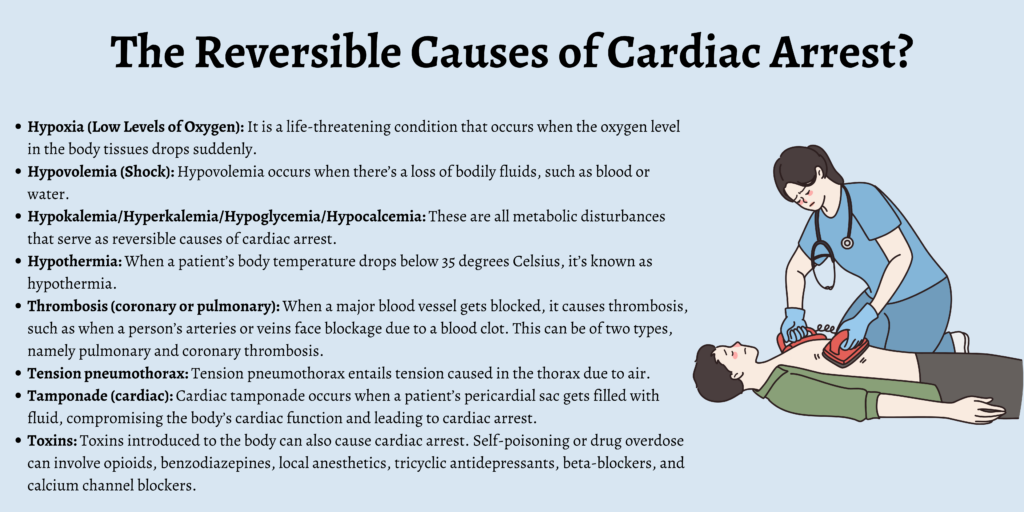
Reversible Causes of Cardiac Arrest – The Four Hs and Four Ts
A cardiac arrest occurs when the heart stops beating in a co-ordinated fashion resulting in the cessation of blood flow around the body.
The main treatment for cardiac arrest is made up of CPR and defibrillation. However first aiders and first responders should also have an awareness of some of the reversible underlying causes of a cardiac arrest.
In some situations it can be possible to identify and treat a reversible cause. Combined with effective CPR and defibrillation, this maximises the chances of the patient surviving the cardiac arrest.
What Are The Reversible Causes of Cardiac Arrest?
The reversible causes of cardiac arrest can be remembered by using the “Four Hs and Four Ts”:
- Hypoxia (low levels of oxygen)
- Hypovolemia (shock)
- Hypokalemia/Hyperkalemia/Hypoglycemia/Hypocalcemia
- Hypothermia
- Thrombosis (coronary or pulmonary)
- Tension pneumothorax
- Tamponade (cardiac)
- Toxins
Hypoxia (Low Levels of Oxygen)
Hypoxia is a life-threatening condition that occurs when the oxygen level in the body tissues drops suddenly. Since oxygen is imperative for the tissues and organs to perform their specific roles, this builds up lactic acid throughout the muscles in the patient’s body.
As a result of this, oxygen loss takes place, which can cause tissue death. Prolonged hypoxia can also harm an individual’s organs, including their brain and heart.
Some of the symptoms related to hypoxia include headache, restlessness, and slow heart rate. Patients experience anxiety and confusion, have shortness of breath, rapid breathing, and heart rate, and witness a blue hue on the lips, skin, and nails.
Proper air circulation should immediately be facilitated in such cases by providing sufficient oxygenation and proper ventilation. Performing CPR can also aid in these circumstances. Once the oxygen levels are restored, the chances of lethal cardiac rhythm can be prevented.
Hypovolemia (Shock)
Hypovolemia occurs when there’s a loss of bodily fluids, such as blood or water. This can happen due to severe vomiting and diarrhea, gastrointestinal bleeding, constant dehydration, extreme sweating, or heavy blood loss.
As a result, the blood flow decreases, and blood and other fluids can’t pass through the blood vessels, making the body enter a state of shock. The patient’s heart weakens in such situations and stops beating eventually.
When a person experiences this condition, they can feel dizzy and sweat excessively. They might also have difficulty breathing, feel their mouth and skin getting dry, and witness their lips and skin turning pale.
Rescue breathing and chest compressions can serve as initial responses for a patient dealing with hypovolemia, but the main issue needs to be treated immediately. This includes administering blood, IV fluids, and plasma based on the problems that cause the loss of fluids.
Hypokalemia/Hyperkalemia/Hypoglycemia/Hypocalcemia
Hyperkalemia, hypokalemia, hypoglycemia, and hypocalcemia are all metabolic disturbances that serve as reversible causes of cardiac arrest. Hyperkalemia refers to the body having abnormally high potassium levels. An excessive amount of potassium can cause a heart attack.
The causes behind hyperkalemia can be endocrine disorders, kidney disease, diabetes, and metabolic acidosis. Hypokalemia can be defined as the opposite of hyperkalemia, wherein the body’s potassium levels decrease.
The treatment for hyperkalemia and hypokalemia depends on whether the potassium levels have decreased or increased. Hypokalemia is usually treated through an infusion of potassium, whereas dialysis is the preferred treatment for hyperkalemia.
Hypocalcemia happens when the blood has low levels of calcium. This can be treated through calcium pills and vitamin C and D supplements.
Hypothermia
When a patient’s body temperature drops below 35 degrees Celsius, it’s known as hypothermia. This increases the chances of one suffering from cardiac arrest, and defibrillation and CPR don’t usually serve as effective treatments for this condition.
Rewarming the patient should be the immediate response in this case. If heat sources and blankets can be used to provide external warmth, CPR can be provided while the warmth gets restored.
Thrombosis (Coronary or Pulmonary)
When a major blood vessel gets blocked, it causes thrombosis, such as when a person’s arteries or veins face blockage due to a blood clot. This can be of two types, namely pulmonary and coronary thrombosis.
Coronary thrombosis happens when a blood clot develops in one of the arteries, thereby preventing blood flow to the heart. This leads to a stroke or myocardial infarction (myocardial infarction).
Pulmonary thrombosis refers to a person’s arteries getting blocked, mostly due to a blood clot. It’s also known as a pulmonary embolism, due to which the heart stops receiving blood.
The treatment for coronary thrombosis usually involves stent placement, angioplasty, or coronary bypass surgery, in some cases. Pulmonary thrombosis can be treated through surgery or medications that involve blood thinners.
Tension Pneumothorax
Tension pneumothorax entails tension caused in the thorax due to air. When air builds up within the body’s pleural space, the mediastinal structures get displaced, and the system’s cardiopulmonary function gets compromised.
Such a condition can cause cardiovascular collapse and even death. Symptoms of tension pneumothorax include rapid breathing, shortness of breath, and chest pain. These symptoms are usually followed by shock.
This can be treated through a chest tube or needle decompression that helps in removing the air buildup from the pleural space.
Tamponade (Cardiac)
Cardiac tamponade occurs when a patient’s pericardial sac gets filled with fluid, compromising the body’s cardiac function and leading to cardiac arrest. This condition is caused due to trauma to one’s chest, such as through inflammation or gunshot wounds.
Cardiac tamponade can either be treated with a thoracotomy, which is a surgical procedure, or through pericardiocentesis, a procedure that helps in removing fluid from the pericardial sac.
Toxins
Toxins introduced to the body can also cause cardiac arrest. Self-poisoning or drug overdose can involve opioids, benzodiazepines, local anesthetics, tricyclic antidepressants, beta-blockers, and calcium channel blockers.
Benzodiazepine overdose is treated through the administration of flumazenil, and opioids overdose is treated with naloxone. Sodium bicarbonate aids in dealing with tricyclic antidepressants, and local anesthetics can be dealt with through benzodiazepines.
Cardiac arrests caused by calcium channel blockers are treated through the administration of calcium chloride.
Although overdose through beta-blockers is more difficult to treat, a patient’s condition can improve through high-dose insulin and glucose, glucagon, phosphodiesterase inhibitors, lipid emulsions, calcium salts, and extracorporeal and intra-aortic balloon pump support.
Although first aiders may not be able to correct some of these reversible causes, it is important that they are considered during the resuscitation attempt whilst high quality CPR is ongoing.
Want to learn more about CPR and resuscitation? Sign up to one of our free online first aid & CPR courses.
When is Cardiac Arrest Reversible?
Cardiac arrest is reversible when CPR is performed on the patient, and a defibrillator is used to shock the person’s heart. This helps in restoring the heart’s normal rhythm within a couple of minutes.
FAQs
What is reverse cardiac arrest?
It’s possible to reverse cardiac arrest when CPR is performed and the normal rhythm of the heart is restored through a defibrillator.
What is the golden minute of cardiac arrest?
A person’s life can be saved if CPR is performed within four minutes.
What is the highest priority in cardiac arrest?
The highest priority in cardiac arrest is high-quality chest compressions.
What are some of the warning signs of cardiac arrest?
Some of the warning signs of cardiac arrest include back pain, shortness of breath, extreme tiredness, nausea, vomiting, and chest pain.
Does a person feel pain during cardiac arrest?
A person could experience chest pain during the initial moments of a cardiac arrest.
Conclusion
Cardiac arrest can occur both due to underlying cardiac diseases as well as non-cardiac causes, including severe infection and toxins. Regardless of the reason behind cardiac arrest, it’s vital to recognize it early on and call for help.
Before seeking professional help, one must appropriately manage the situation so that proper intervention can take place. Go through the reversible causes of cardiac arrest listed above so that you can help a person if the situation arises.