First Aid for Pain: Pain Assessment and Management
If you’ve ever experienced being in an accident, you may remember responders asking if you were in pain. It’s one of the first things they ask to know if you’re injured.
In the medical field, this type of questioning is a systematic way to help someone in pain right away. Its goal is to assess the pain that the victim experiences so that they can provide care and pain relief.
How Does Pain Work?
Pain is a sensation that happens when our pain receptors activate in response to a stimulus. Experts believe it is your body’s way of alerting you that something is wrong.
For instance, if you accidentally put your hands on a hot stove, the pain receptors activate, and your brain will cause a muscle contraction (reflex) to pull your hands away from the stove.
However, the pain caused by these experiences varies from person to person. We call this phenomenon the “pain threshold”—it’s why some pain is severe to some people but minimal to others.
Pain Assessment and Management
While you can consider pain highly subjective, it’s real and it can affect the mental and emotional conditions of patients. This is where pain assessment and management come in.
Pain assessment is a broad medical concept. It’s when doctors make a clinical judgment based on observation, an interview, and the context of the pain that the patient experiences.
Evaluating pain is crucial in situations that involve injuries or grave illnesses. It’s a vital component of managing discomfort to create a proper treatment plan.
What Are the Steps of Pain Assessment?
Medical practitioners follow a protocol when assessing pain and discomfort. This protocol involves a series of steps to help figure out what’s causing the pain and give the right care. The basic goal is to identify the source of the pain in order to help relieve pain in the patient.
Step 1: Rating Pain
In evaluating the discomfort a patient experiences, physicians usually ask them to describe the degree of pain. Through this, they’ll be able to quantify the data and determine interventions.
In measuring discomfort, they use pain rating methods like FLACC, WILDA, or PQRST. These tools involve numerical, verbal, and observational approaches to pain assessment.
These tools will determine the pain history, location, and intensity. It will enable the doctor to analyze and comprehend the nature of their patient’s pain.
Step 2: Provide Relief
After a successful rating, the doctor will recommend or administer pain-relieving treatments. They may provide analgesia or other pain relievers to alleviate pain.
As mentioned earlier, acute pain can affect both the emotional and mental conditions of patients. Providing relief will allow the body to focus on healing.
It’s particularly crucial for patients with terminal conditions, as pain can hinder them from doing things they enjoy. In such cases, managing pain is the only way to improve their quality of life.
Step 3: Report and Document
The doctor will record and document all the data gathered from the pain assessment. They’ll use the information to create a holistic treatment plan to address the patient’s condition.
Properly documented pain assessments will improve communication between clinicians. It’ll ultimately help improve the quality of pain management that patients receive.
However, pain assessment and management don’t end with reporting and documentation. It’s an ongoing process of rating, relieving, and recording until full recovery is achieved.
Different Rating Scales
Doctors use different rating scales when assessing pain and discomfort. The scale will depend on the patient’s age, condition, and cognitive abilities.
1. Numerical Rating Scale
A numerical rating scale involves assigning a numerical value to the pain you’re experiencing. The scale typically ranges from 0 (no pain) to 10 (severe pain).
This scale is good for adults and kids over the age of six who know what orders and ranks are. This detail is important for the accuracy of the assessment.
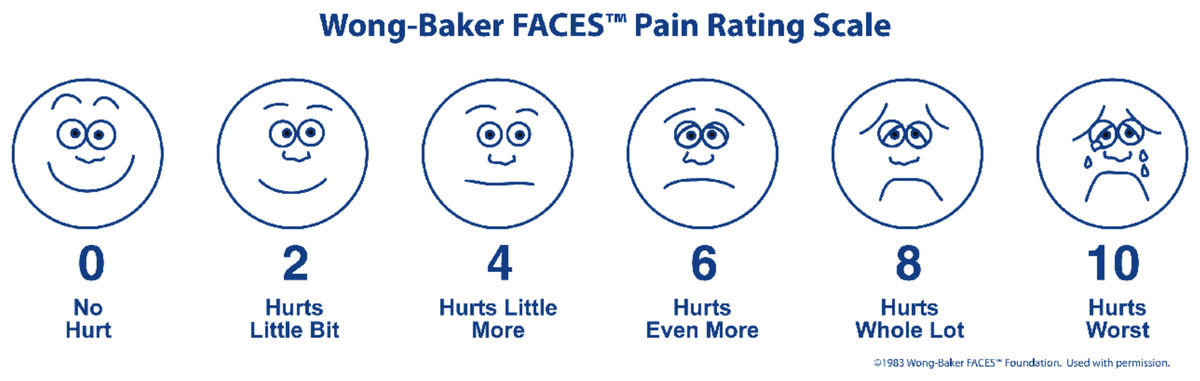
2. Wong-Baker Pain Scale for Adults and Children
The Wong-Baker pain scale is used for patients ages 3 to 18. The purpose of this tool is to help children effectively communicate the discomfort they’re experiencing.
The scale is a series of faces, beginning with a happy face (no pain) to a crying face (worst pain imaginable). Doctors will ask the patient to point at the picture describing their feeling.
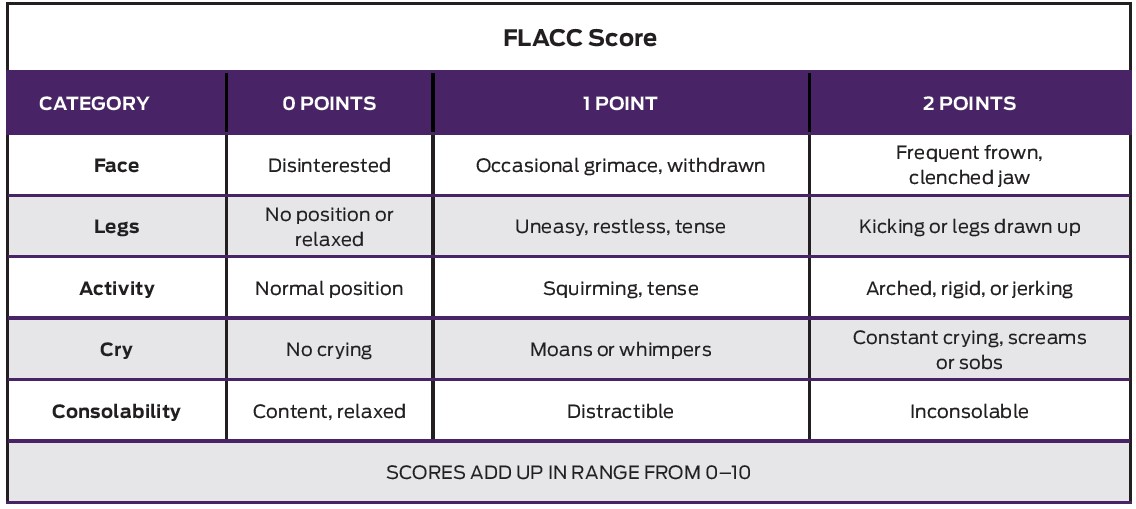
3. FLACC
FLACC stands for face, legs, activity, cry, and consolability. It’s a pain rating tool based on the behaviors and physical symptoms of the patient.
This method has five checkpoints corresponding with the five areas of observation. The doctor will observe and rate them from 0 (relaxed) to 2 (agitated).
Physicians commonly use this scale for patients who can’t report the intensity of the discomfort themselves. It’s for children and adults with cognitive and verbal impairments.
4. WILDA
WILDA stands for words, intensity, location, duration, and aggravating/alleviating factors. This tool offers a direct and concise approach to assessing chronic and acute pain.
This approach, however, requires a patient that can communicate as it involves a conversation with the physician. It’s a combination of numerical ratings and self-report descriptions of pain.
5. WHO Pain Ladder
The World Health Organization proposed a strategy for pain assessment and relief called the WHO analgesic ladder. It’s a tool physicians use specifically to quantify pain for cancer patients.
There are three steps to this ladder. All three levels relate to the intensity of the pain and their corresponding pain management.
Here are the levels of the WHO analgesic ladder:
Level 1: Mild Pain
Mild pain is the lowest level of the ladder. It involves discomfort that doesn’t require therapeutic and prescription medication to relieve.
Level 2: Moderate Pain
This level refers to temporary discomfort. However, the degree of pain can interfere with the patient’s daily activities, so physicians prescribe weak analgesics.
Level 3: Severe Pain
This stage involves acute and persistent discomfort. The pain can be unbearable, so it requires analgesics and therapeutic medications.
PQRST!
No article about pain assessment would be complete without mentioning the PQRST mnemonic, which is a useful tool for figuring out how much pain someone is in when there is a medical emergency.
This strategy describes a broader approach to first response, but it involves a critical pain assessment step. A responder following PQRST will make use of one of the above pain rating scales during the “S” step of the assessment.
For a more detailed look at this method, we have a whole post dedicated to the PQRST method.
What Does PQRST Stand For?
PQRST is a pain assessment method that stands for:
- Provocation or palliation
- Quality
- Region or radiation
- Severity
- Timing
Final Thoughts
Pain assessment is a way for patients and doctors to work together. It enables patients to share their experiences and receive the appropriate care and medication they need.
Properly administered pain management is pivotal to the overall well-being and healing of the patient. To this end, physicians must use different methods to suit the needs of every individual.






This is absolutely electric
Glad that you liked it 🙂
I really enjoyed this. Thank u
Glad you found it helpful!
very helpful for CNA and nurses
good and refreshes the brain